Opportunity
Medicines are the commonest intervention used in healthcare. Research regularly shows that of all iatrogenic harm that occurs, up to 38% are related to medicines and these are known as adverse drug events (ADE). As part of Waitemata DHB’s promise to its community which is best care for everyone and the delivery of care which is safe, continuously improving and among the best in the world, we need robust data to help:
-
inform how safe medication systems currently
-
identify areas for further improvement
-
track progress over time
Despite the need for information to monitor medication safety, a major challenge has been the resource required to manually collect data in already busy healthcare environments.
Data is typically only collected for specific projects over short periods of time and cannot sustainably or routinely be maintained for prolonged periods.
Our aim was to develop a practical and sustainable yet meaningful surveillance dashboard to better monitor medication safety and its progress.
Using the MSSA-AH® findings (Medication Safety Self-Assessment for Australian Hospitals) as the platform, we identified and selected nine key measures:
- ADEs (adverse drug events) per 100 discharges
- % of patients who recalled hospital staff telling them about medication side effects to watch for
- Medication safety self-assessment (MSSA®)) % score
- Health and Disability Services (H&DSS) and Medsafe certification (pass/fail)
- % of discharges where eMedRec performed
- % of drugs prescribed by quicklist/ pre-set
- % of drugs screened for safety by Pharmacy before administration
- % of nurses observed to completely comply with administration bundle
- Medication incidents voluntarily reported per 100 discharges
To reduce the need for manual data collection, where possible, metrics where data can be obtained from routinely collected administrative data and/or electronically sources were favourably selected. The data for the metrics are obtained from:
- coded patient admission data (eg national minimum dataset (NMDS))
- Health Round Table
- Patient and Whānau Centred Care Standards (PWCSS)
- incidents and complaints reporting database (ie RiskPro)
- nationally collected datasets (eg HQSC national inpatient experience survey)
- electronic medication systems such as:
- electronic prescribing and administration
- electronic medicines reconciliation
- pharmacy dispensing data
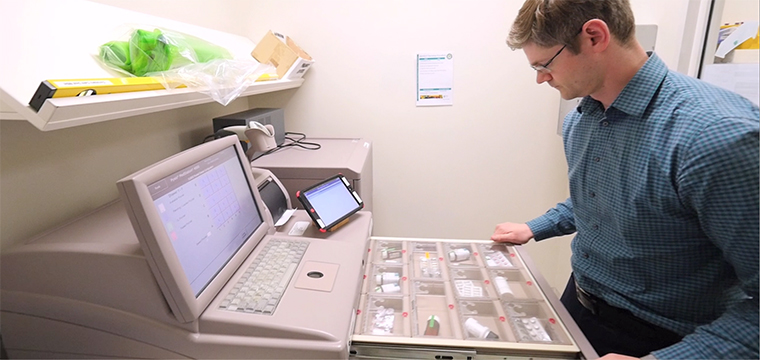
- software for automated dispensing cabinets (ADC)
The data is presented as a scorecard/dashboard on an A3 double-sided report to the Medication Safety Group once every quarter and represent in both graphic and table formats.

Medication Safety Surveillance Dashboard (Jul 2017)
At a practice level, the medication safety surveillance dashboard is now routinely used at Medication Safety Group to monitor high risk areas, inform improvement and track progress of introduced initiatives over time. Because the data sources listed above have either already been routinely collected for administrative or reporting basis or they are from digital systems which automatically collect and store detailed data and generate metadata (i.e. data about the data); it minimises the need for manual data collection.
The primary metric for medication safety measurement and monitoring has focused on detecting and measuring ADEs or subsets thereof. But just as health means more than the absence of disease, safety means more than the absence of harm and contemporary research in the field of safety measurement (e.g. Safety I to Safety II concept) recognise the need to also include other key metrics for more comprehensive and balanced assessment. For the first time in NZ, we have developed a dashboard/scorecard which monitors important facets of medication safety without the need for extensive manual data collection. By providing access and visibility of data on medication safety, it actively engages both clinical and managerial staff and provides the means for further monitoring. We are still in the early stages of developing the medication safety surveillance dashboard but are continuing to look for ways to improve it. For example, we have already started to extract data from our ePA system to monitor omitted/missed medication doses and when they occur; data not previously obtainable without significant manual input.

As our surveillance and digital medication systems mature we will continue to explore how they can be better interrogated, linked to other datasets and used to inform improvement and safeguard patients.
Working Group
- Jerome Ng, i3 Lead Advisor Improvement Research + Informatics
- Penny Andrew, Director of i3
- Marilyn Crawley, Chief Pharmacist
- Wynn Pevreal, Medication Safety Pharmacist
- D Croft
- Delwyn Armstrong, i3 Head of Analytics
- Andrew Brant, Chief Medical Officer
- Jocelyn Peach, Director of Nursing + Midwifery